This transcript has been edited for clarity.
Kenneth W. Lin, MD, MPH: I'm Dr Kenny Lin, family physician and associate director of the Lancaster General Hospital Family Medicine Residency. I'm here today with Dr Alka Gupta, who is on the board of directors of the American College of Lifestyle Medicine (ACLM), to talk about lifestyle medicine in primary care. Dr Gupta practices in Washington, DC, and has been one of the leaders at the forefront of the lifestyle medicine movement. In fact, I saw my personal physician earlier today, and he mentioned that he had attended the ACLM virtual conference this year and was very enthusiastic about lifestyle medicine. A great coincidence, and a perfect opportunity to talk about this.
Let's start with the basics. When you tell your patients and colleagues that you have training and expertise in lifestyle medicine, how do you explain what that is and how that can help them?
Alka Gupta, MD: With patients, we're usually talking about what it is that they want from their health. So I tie it to their goals. Are they looking to live longer, or live better? Sometimes we talk about chronic illnesses that can be prevented or even reversed by optimizing nutrition, physical activity, and how we deal with everyday challenges. If their goal is something else, then we might be showing that person how working within one of those lifestyle medicine tenets can help them achieve that goal.
For clinicians, we know that lifestyle medicine has a massive impact on a person's health — short term, day to day, and long term. That makes lifestyle medicine relevant to everyone alive. Therefore, it's relevant to all clinicians. It doesn't mean that everyone needs to know everything about it. But I think there's an increasing realization that this is part of medicine.
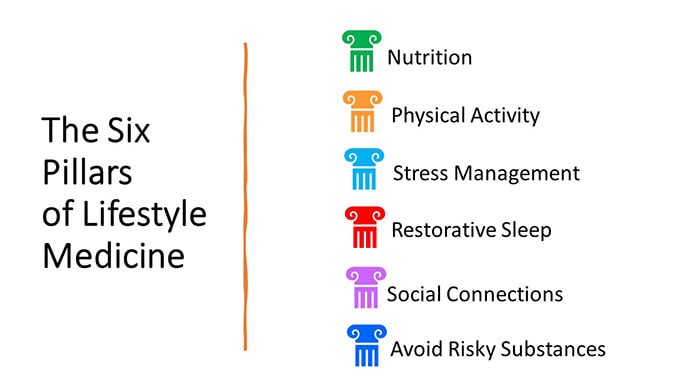
Lin: Part of the attraction of lifestyle medicine is that clinicians are encouraged to practice what they preach. The six pillars of lifestyle medicine should be central to their own lifestyles and could reduce their risk for burnout. Could you tell us about the six pillars that are the core of lifestyle medicine?
Gupta: The six pillars that we promote awareness of in lifestyle medicine are nutrition, physical activity, stress management, restorative sleep, social connectedness, and avoiding risky substances that can actively harm your health.
Lin: The pillars that intrigue me the most are stress management and social connections, because they're obviously really important to well-being, but I don't talk about them as often as nutrition or physical activity. I've often felt that those things aren't really under my control. How do you help patients better manage their own stresses and spend more quality time making social connections?
Gupta: It's hard, especially now. Many of us live and work in a hybrid way. I have seen a lot more isolation in the past few years than there was earlier, which makes all of those things harder.
Stress tends to be a nebulous topic. My first goal is to help a person, whether it's a patient or someone else, understand whether they're having a stress reaction that could be negatively impacting their health. Many people are working or living in stressful situations, and we might not even be aware of the toll that is exacting on our health. Once we recognize that, I find that the rest of the conversation becomes a little bit easier.
Changes are easier if you have a bit of community around you. It could be a small community — a couple of family members, friends, or colleagues. I find it a lot easier to get physically active if I'm doing it with somebody else or taking a class that connects me to other people. I'm more excited about it..
Lin: Medical training isn't always conducive to living a healthy lifestyle. I can remember being on call and grabbing whatever there was to eat at the hospital cafeteria and neglecting exercise. Is ACLM looking at changes we could make to training and medical practice that could improve the situation?
Gupta: In general, we've seen improvements in the structure of medical education across the board. For the good health of patients, we also need to be paying attention to the health of our teams and healthcare workforce. We see clinicians leaving the profession in droves, which is a massive issue. We need to be able to take care of our own health by addressing those six pillars for ourselves. A lot of work must still be done in this area.
Lin: I was looking at the ACLM website. The organization has experienced a great deal of growth since it was founded more than 20 years ago. How does it look for the next 20 years? Do you see lifestyle medicine as remaining anchored in primary care or evolving into a subspecialty of primary care, like sports medicine?
Gupta: ACLM has changed a lot. It started out as a physician-led group that was quite small and grassroots. We've led a major push to educate clinicians — both in training and after training — on how lifestyle medicine can be feasibly implemented into practice.
As far as whether lifestyle medicine should be anchored in primary care or elsewhere, we need to transform health at a population level, a national level, and even at the individual level. We need depth. Primary care will always be an important entry point, perhaps the most important. But we can't rely on primary care clinicians to do it all. We need other health professionals: nutritionists, registered dietitians, exercise physiologists, fitness specialists, and behavioral health specialists. We need to bring them in with an eye toward a care delivery system that is connected, coordinated, and communicates well and wraps itself around a patient. So, although it's an amazing anchor (and that's why I'm in primary care), we can't rely solely on primary care. Lifestyle medicine should be incorporated into all specialties. If an endocrinologist is diagnosing diabetes, nutrition has to be part of that conversation so the patient knows what's within their control in their diabetes management.
Lin: Do you have a sense of what percentage of your members are in primary care vs other subspecialties?
Gupta: I don't have the figure in front of me, but we have a lot of specialty representation. Cardiology is one of the more highly represented specialties, which is great. Much of what cardiologists do is prevention, so it has a perfect place in lifestyle medicine. If we're talking about advanced therapeutics or diagnostics, even invasive tests, like left heart catheterization and stent placement, it's great that the same clinicians are providing the message about prevention.
Lin: Purely in a cynical sense, if you're a cardiologist promoting lifestyle medicine, you're trying to reduce a lot of your business. Hopefully patients won't need so many invasive procedures, such as revascularization, if we can prevent disease in the first place.
ACLM recently published an expert consensus statement about integrating lifestyle medicine into primary care practice. Many of the services are very time intensive. In terms of what we can do in primary care today, could you talk about shared medical appointments and other ways that family physicians and general internists can offer lifestyle medicine in their practices?
Gupta: We spend a lot of time trying to circumvent that exact problem. With one practitioner and one patient, you can't address everything in one visit, including 20 minutes teaching them how to have a balanced meal or what type of physical activity is best for them. So, we help practices use shared medical appointments, where you bring in multiple patients at one time. One benefit is that you can bring in resources that might not otherwise be a covered benefit for some patients. For example, you might bring in a registered dietitian or psychologist or other practitioners that patients might not always have ready access to. You can provide that education in a group environment that's also billable. It's more feasible for a practice to reach more patients with that information, and patients also love shared appointments because they get to learn from each other.
Lin: Are there any take-home points about lifestyle medicine for family physicians that we haven't already talked about?
Gupta: The key catalyst for me was when I started realizing how much chronic illness can actually be prevented in the first place and then how much can be stalled or delayed, even after the onset. Once I became aware of that, it was a lot more important to me to incorporate that into my everyday practice. That's the most important thing to know.
Clinicians are intrinsically motivated to do the best for their patients. You tend to find ways and resources to offer the things that you may not have the capacity to do yourself. ACLM has a treasure trove of resources that practices can avail themselves of, including a great handout for patients, "6 Ways to Take Control of Your Health." ACLM is an amazing community to get involved in.
Lin: Many clinicians are ready to receive this message. Thank you so much for taking the time to speak with me today about lifestyle medicine.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Image: Medscape
Medscape Family Medicine © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Primary Care, Meet Lifestyle Medicine - Medscape - Dec 18, 2023.










Comments