This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I'm Dr Matthew Watto, here with my great friend, Dr Paul Nelson Williams. We're going to talk about the treatment of the vasomotor symptoms of menopause, from our podcast with Dr Monica Christmas.
Let's start off with nonpharmacologic therapy, which some people may think is boring but I think is important. And as America's primary care physician, this is right in your wheelhouse.
Paul N. Williams, MD: I don't think people think it's boring. The struggle is that you worry whether you have enough time, and sometimes it feels clichéd, but it turns out that a lot of the stuff that we recommend in primary care also helps mitigate the vasomotor symptoms of menopause, like sufficient sleep ( I know — easier said than done) and getting routine exercise. Dr Christmas emphasized that weight loss can go a long way toward mitigating some of the symptoms as well. These are the conversations you're already having in the primary care setting, so you're well suited to at least reinforce those points or use this as an additional carrot to move the needle because it will actually help with their symptoms.
Watto: And those things are easier to access than cognitive-behavioral therapy or hypnosis, which do actually work. What about medications that are not hormones?
Williams: We covered a lot of options. In terms of the SSRIs, paroxetine is the one that is FDA approved for the vasomotor symptoms of menopause. We had a conversation about the potential side effects, but you use this at a lower dose than you would for a depression or anxiety, which is important to know. Among the SNRIs, there is venlafaxine and gabapentin, and the new kid on the block, fezolinetant, which is also nonhormonal. We're seeing it being direct-to-consumer advertised now, which is very exciting. Matt, remind me — how are we using it?
Watto: They tested this in women who had moderate to severe hot flashes. It worked better than placebo — something like two fewer hot flashes per day. The placebo group had seven hot flashes daily and the treatment group had five. You do have to monitor liver enzymes at 0, 3, 6, and 9 months for the first year of treatment. In some of the other trials, there was a little bit of liver enzyme elevation, but it's more that other drugs in this class that have been tried in the past had more significant liver enzyme elevations. That's why they're watching out for that. So I think this is something you can consider. It's certainly being advertised, so patients are going to ask about it.
There is hormone therapy, and probably the pendulum has swung too far away from using that. So, tell us, what is it used for? Who is it approved for?
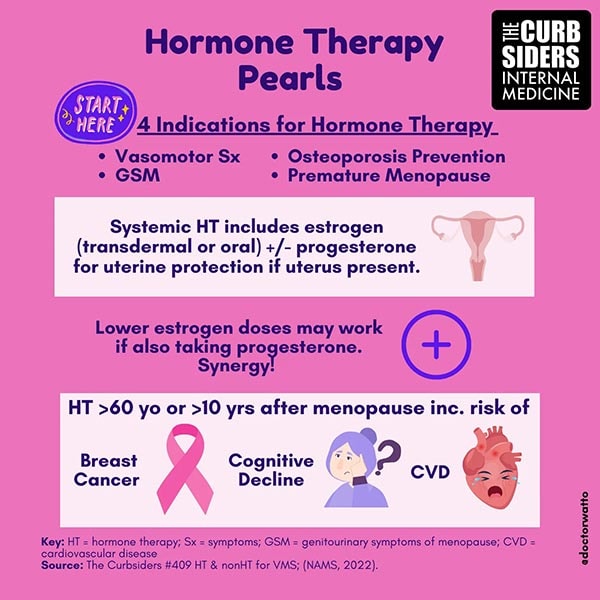
Williams: We've gotten very gun-shy about using hormone therapy, and I understand the reasons. It's approved for the vasomotor symptoms of menopause, the genitourinary symptoms of menopause (and there are topical preparation options for that as well), osteoporosis prevention (which is one I forget about but does exist), and premature menopause, which is menopause before the age of 40 or surgical menopause. The idea is that you treat with hormone therapy until about age 52 (which is thought to be the natural age of menopause), and then you would stop it and patients would do okay.
Watto: You would continue it at least that long; you don't have to stop at any specific point. You use the lowest dose for the shortest amount of time and try to take them off. But Dr Christmas did mention that some people are chronic hot flashers and might need to stay on therapy for a long time.
Williams: She framed it as shared decision-making. There are patients who understand the risks and are still happy to continue because they feel so much better with the medication than without it. That's a very reasonable approach, as long as they are educated about it and we document it well.
Watto: And they're still being monitored with regular breast cancer screening. If they develop a blood clot, that would probably be a reason to stop hormone therapy, or if their cardiovascular risk changes. If they are less than age 60 or less than 10 years since menopause and they're having really severe symptoms, and they've tried other things, hormone therapy may be reasonable. Dr Christmas told us that she often will start with a medium dose of estrogen because, in her experience, it tends to work for most people. If you start at too low a dose, the patient might think it's not going to work and give up on the therapy.
Click on the link to listen to the full podcast with Dr Christmas, because it was really a masterclass with somebody who helps write the guidelines and knows everything. She has a lot of great scripts on how to counsel your patients. I highly recommend that people check it out.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Image: The Curbsiders
© 2023 WebMD, LLC
Cite this: Matthew F. Watto, Paul N. Williams. Dr Christmas on Managing Menopausal Symptoms - Medscape - Dec 05, 2023.











Comments