Re: Hyperbaric Oxygen Therapy for Traumatic Brain Injury: Promising or Wishful Thinking?
To the Editor:
In July of last year, the European Society of Medicine published our literature review on the efficacy of hyperbaric oxygen therapy (HBOT) in the treatment of traumatic brain injury (TBI).[1] This comprehensive review encompassed all human studies conducted over the past 54 years and provided recommendations based on the level of evidence and classification.
In his commentary, titled "Hyperbaric Oxygen Therapy for Traumatic Brain Injury: Promising or Wishful Thinking?," Andrew N. Wilner, MD, did not differentiate between the evidence levels and recommendations for acute and chronic TBI, which were clearly delineated. We regret he found the most comprehensive review to date unwieldy. Perhaps that is why he focused primarily on chronic TBI and overlooked our primary recommendation and suggested the review was a disservice to desperate patients.
In acute TBI settings, high-quality randomized controlled trials have clearly demonstrated a reduction in mortality with varying functional outcomes. Unfortunately, in his critique, Dr Wilner omitted or failed to read that we have proposed a Class 2a recommendation for the use of HBOT in acute TBI while acknowledging the need for further research to determine the optimal protocol for improving functional outcomes.
One of the major challenges in HBOT human studies has been establishing an appropriate control group.[2] As patients can sense changes in environmental pressure due to the need for pressure equalization, the control group has typically been exposed to increased pressure, usually around 1.3 absolute atmospheres (ATA). However, it's essential to note that exposure to higher environmental pressure is in itself an active biological intervention. Recently, MacLaughlin and colleagues reported that hyperbaric air at 1.27 ATA with an oxygen partial pressure of 0.26 can mobilize stem cells.[3] Therefore, pressure changes cannot be considered as a suitable sham or placebo.
The upcoming HOT-POCS trial,[4] recommended by Dr Wilner to answer this question, also faces the same limitation which he failed to mention. Even though the sham group will breathe oxygen at an absolute partial pressure of 0.21 ATA, the daily exposure to 2 ATA will still have significant physiological effect. Furthermore, during compression and decompression (lasting at least 23-30 minutes), the sham group will be exposed to hyperbaric oxygen with a partial pressure ranging from 0.21 to 0.42 ATA. Unfortunately, this sham method has been suggested and used previously, and HOT-POCS doesn't deviate from this approach.[4]
Our group has recently established a more appropriate sham intervention that has no significant biological effect.[5] In this method, subjects are exposed to 1.2 ATA for 5 minutes during compression, followed by normobaric air (1.01 ATA, 0.21 oxygen partial pressure) for the rest of the session and decompression. This approach has demonstrated effective blinding in three randomized controlled trials, both in healthy[5] and pathologic conditions,[6] including pediatric post-concussion syndrome.[7] The neuroplasticity and neurocognitive beneficial effects induced by HBOT, which Dr Wilner denies occurs, were clearly demonstrated in all of those randomized, sham-control clinical studies.[5,6,7]
Dr Wilner and his colleague Dr Conidi maintain that there is insufficient justification to recommend HBOT, but they do agree that the currently available standard therapy is ineffective. It is worth emphasizing that many of the recommended therapeutic modalities, such as cognitive rehabilitation, pharmacotherapy, or physical therapy, have less quantity and quality of evidence compared to HBOT. Moreover, most of these modalities have not been investigated in multicenter standardized studies. Interestingly, most neurological societies do not provide specific guidelines for the therapy of chronic TBI. For instance, patients with chronic TBI are often recommended various neurostimulants, including amantadine, selective serotonin reuptake inhibitors, tricyclic antidepressants, central stimulants (eg, methylphenidate), modafinil, and donepezil.
However, well-powered studies have never been conducted to validate their use in patients with TBI, leaving uncertainty regarding the role of these agents in therapy.[8,9] Current practice often relies on physician consideration of patient-specific factors, which may lead to the use of appealing but unproven therapies, whether in the treatment of epilepsy, headache or TBI, as Dr Wilner mentions.
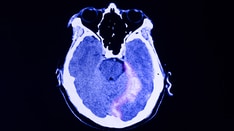
Many previous clinical trials of HBOT have significant methodological issues.[1] Objective measures, brain imaging, exclusion of comorbidities, and careful patient selection are crucial aspects in TBI research. Studies that have incorporated these elements into their protocols provide a more accurate assessment of the effects of HBOT in chronic TBI. Nevertheless, we concur that further sham-controlled trials are needed to optimize both patient selection and HBOT protocols in TBI and as mentioned, it should include the appropriate sham
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Hyperbaric Oxygen Therapy for Traumatic Brain Injury: Evidence-Based Medicine - Medscape - Nov 08, 2023.









Comments