This transcript has been edited for clarity.
I'm Dr Rachel Rubin, a urologist with fellowship training in sexual medicine.
It's important for doctors to ask about erections. Not only do our patients and their partners care about them, but they are a marker for overall health. I mean it. Penis problems are very common and are an early sign that patients could have a cardiac event. Think about it: Clogging the arteries of the heart is called a heart attack; clogging the arteries to the penis is a penis attack, or as doctors like to call it, erectile dysfunction.
The arteries to the penis are only 1 mm in diameter. They develop plaque and clog the circulation long before the 3-mm cardiac arteries. So, it's very important for primary care doctors to talk to their patients about erection health. And I'll be honest: It's easier to talk to patients about how lifestyle is affecting their penis health than it is to discuss how lifestyle affects longevity or prevents cancer. I get a lot of men to quit smoking because I tell them what it's doing to their penises.
It can be challenging for doctors and patients to talk about penises. It doesn't come naturally for many of us. If a 20-year-old comes in to my office with his 85-year-old grandfather and they both say their penises aren't working, how do you figure out what's going on? Do they even have the same thing wrong with them?
Here's a fun and helpful tool that I use in my office. It's called the Erection Hardness Score (EHS). It was developed around the time that Viagra came out, in 1998. It's been game-changing for me to get patients more comfortable talking about their erection issues.
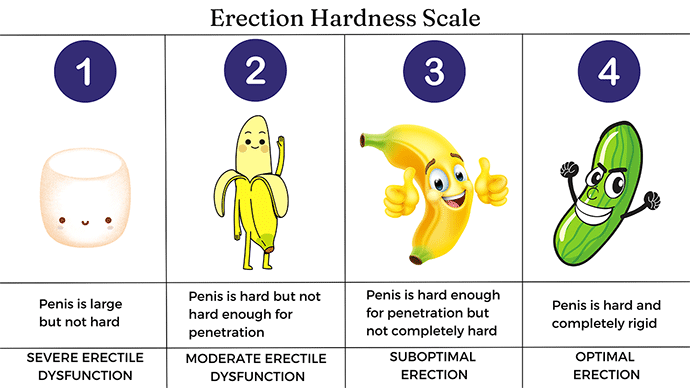
I tell them it's a 4-number scale. A "1" is no erection at all. A "2" is when it gets harder and larger, but it's not going to penetrate. A "3" will penetrate, but it's pretty wobbly. A "4" is that perfect cucumber–porn star erection that everyone is seeking. I have the patient tell me a story. They may say, "When I wake up in the morning, I'm at a 2. When I stimulate myself, I can get up to a 3. When I'm with my partner, sometimes I can get up to a 4."
This is really helpful because they can talk in numbers. And after I give them treatments such as lifestyle changes, sex therapy, testosterone, a PDE5 inhibitor such as Viagra or Cialis, or an injection, they can come back and tell me how the story has changed. I have an objective measure that shows me how the treatment is affecting their erections. Not only do I feel more confident having those objective measures, but my patients feel more confident in the care that they're getting, and they feel more comfortable talking to me about the changes. So, I encourage all of you to bring that EHS tool into your office. Show it to patients and get them more comfortable talking about erections.
I'll talk about treating erectile dysfunction in a future video.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Image: Rachel Rubin, MD
Medscape Urology © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: The Easy Way to Talk About Penises - Medscape - Nov 10, 2023.












Comments