This transcript has been edited for clarity.
Dear colleagues, I'm Christoph Diener from University Duisburg-Essen, and this month I will report on seven studies that were published in October 2023.
Hearing Loss and Dementia
Let me start with hearing loss as a risk factor for cognitive impairment and the development of dementia. This has long been known, but would it work if you improve hearing function? This has been studied in the randomized ACHIEVE study published in The Lancet. The investigators randomized 977 patients, with a mean age of 77 years, with untreated hearing loss and low cognitive impairment.
They either received a hearing device or education. After 3 years, there was no difference in global cognitive function, measured by a battery of neuropsychological tests. There was, however, a significant benefit of hearing devices in patients at increased risk for cognitive decline.
PD Risk and Common Drugs
My next study, published in Neurology, deals with an interesting question: namely, are there drugs that are associated with a decreased or increased risk for Parkinson's disease? This is a cohort study of the entire Norwegian population between 2004 and 2019, with 600 million prescriptions.
The study population was 3.2 million people in Norway, of whom 15,850 developed Parkinson's disease. Associated with a lower risk for Parkinson's disease were drugs that act on the renin-angiotensin system, systemic administration of corticosteroids, and vaccines.
An increased risk for Parkinson's disease was associated with drugs that are usually given to treat prodromal symptoms of Parkinson's disease, such as constipation, incontinence, and depression. This should perhaps encourage us to do prospective studies with drugs that act on renin-angiotensin system — for example, antihypertensive treatment — and see what happens.
Thrombectomy and Ischemic Conditioning for Ischemic Stroke
The third study deals with the benefit of endovascular thrombectomy in patients with large ischemic infarcts. We were always afraid to treat these patients because we were afraid of bleeding into the ischemic area after successful recanalization. The TENSION study, published in The Lancet, randomized 253 patients with occlusions of the large arteries and large ischemic strokes, defined as ASPECTS score of 3-5 within 12 hours.
Thrombectomy compared with medical treatment was significantly more effective than medical therapy for the functional endpoint. This means, together with the two studies that were published earlier this year, we have now three randomized trials that clearly show the benefit of thrombectomy in people with large ischemic stroke and no increased risk for bleeding into the ischemic area.
My next topic is remote ischemic conditioning, which is used in myocardial infarction. Last year, there was a study published in China showing that remote ischemic conditioning with ischemia at the upper extremities improves outcome after ischemic stroke.
This study was replicated in Denmark, with 1500 patients randomized within 4 hours. These patients received five cycles of 5 minutes of ischemia of the upper extremities twice daily for 7 days or sham. Compared with the control group, there was no difference in functional outcome. Therefore, I really doubt whether remote ischemic conditioning works in ischemic stroke.
Anticoagulation Post-ICH
My next study deals with the question what to do with patients with atrial fibrillation who are anticoagulated and have intracranial bleeding. These patients have a high risk for ischemic stroke and would need anticoagulation, but they also have an increased risk for bleeding. What is the benefit or risk?
This is a single patient-based meta-analysis of four small trials, a so-called Cochrane study published in The Lancet Neurology. The investigators looked at 412 patients and found no difference for stroke or death in patients receiving anticoagulation compared with people who did not receive anticoagulation.
This was most probably not an adequate endpoint because if you look at ischemic events, and in particular ischemic strokes, there was a clear benefit of initiating anticoagulation — again, with only a small increased risk for intracerebral or intracranial bleeding. We will learn more when the ongoing, larger, randomized trials are finalized.
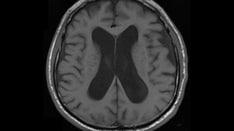
My next study deals with radiologically isolated syndrome risk. This is a predictor of multiple sclerosis. These are people who have MS signs on MRI but no symptoms. Last year, a study was published that showed that glatiramer acetate has a benefit in these patients by delaying the time until the first clinical manifestation of multiple sclerosis.
This was now studied with teriflunomide in 124 patients and published in JAMA Neurology. The study showed that, in these patients, treatment with teriflunomide compared with placebo delayed the time until the first clinical manifestation of MS. There was no difference, by the way, in the number of newly developed MS loci on MRI.
My last study, published in the Journal of Headache and Pain, deals with the question of how common triptan nonresponders are. We have two new classes of migraine drugs for treatment: gepants and ditans. These drugs are promoted by companies for patients who are so-called nonresponders to triptans.
The German Headache Society looked in its database at more than 2200 patients to see how often patients are not responding to a triptan. They found out that 42% were failures to one triptan, 13% to two triptans, and only 4% to three triptans. This basically shows that nonresponders are almost nonexistent. This would be particularly true if the most effective treatments are used; these are rizatriptan and eletriptan.
Dear colleagues, I think October was a fascinating month for neurology. I'm Christoph Diener from the Medical Faculty of the University Duisburg-Essen. Thank you very much for listening and watching.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Medscape Neurology © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Fall Updates in Dementia, Parkinson's Disease, and Stroke - Medscape - Nov 22, 2023.










Comments