This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
Let's assume, for the sake of argument, that I am a healthy 43-year old man. Nevertheless, I am interested in getting my vitamin D level checked. My primary care doc says it's unnecessary, but that doesn't matter because a variety of direct-to-consumer testing companies will do it without a doctor's prescription — for a fee of course.
Is that okay? Should I be able to get the test?
What if instead of my vitamin D level, I want to test my testosterone level, or my PSA, or my cadmium level, or my Lyme disease antibodies, or even have a full-body MRI scan? All of these tests are available from a variety of direct-to-consumer testing companies. If I am willing to pay, should I be able to get those too?
These questions are becoming more and more common, because the direct-to-consumer testing market is exploding.
We're talking about direct-to-consumer testing this week, thanks to this paper: Policies of US Companies Offering Direct-to-Consumer Laboratory Tests, appearing in JAMA Internal Medicine, which characterizes the testing practices of direct-to-consumer testing companies.
But before we get to the study, a word on this market. Direct-to-consumer lab testing is projected to be a $2 billion industry by 2025, and lab testing megacorporations Quest Diagnostics and Labcorp are both jumping headlong into this space.
Why is this happening? A couple of reasons, I think. First, the increasing cost of healthcare has led payors to place significant restrictions on what tests can be ordered and under what circumstances. Physicians are all too familiar with the "prior authorization" system that seeks to limit even the tests we think would benefit our patients.
Frustrated with such a system, it's no wonder that patients are increasingly deciding to go it on their own. Sure, insurance won't cover these tests, but the prices are transparent and competition actually keeps them somewhat reasonable. So, is this a win-win? Shouldn't we allow people to get the tests they want, at least if they are willing to pay for it?
Of course, it's not quite that simple. If the tests are normal, or negative, then sure — no harm, no foul. But when they are positive, everything changes. What happens when the PSA test I got myself via a direct-to-consumer testing company comes back elevated? Well, at that point, I am right back into the traditional mode of medicine — seeing my doctor, probably getting repeat testing, biopsies, etc., — and some payor will be on the hook for that, which is to say that all of us will be on the hook for that.
One other reason direct-to-consumer testing is getting more popular is a more difficult-to-characterize phenomenon which I might call postpandemic individualism. I've seen this across several domains, but I think in some ways the pandemic led people to focus more attention on themselves, perhaps because we were so isolated from each other. Optimizing health through data — whether using a fitness tracking watch, meticulously counting macronutrient intake, or ordering your own lab tests — may be a form of exerting control over a universe that feels increasingly chaotic. But what do I know? I'm not a psychologist.
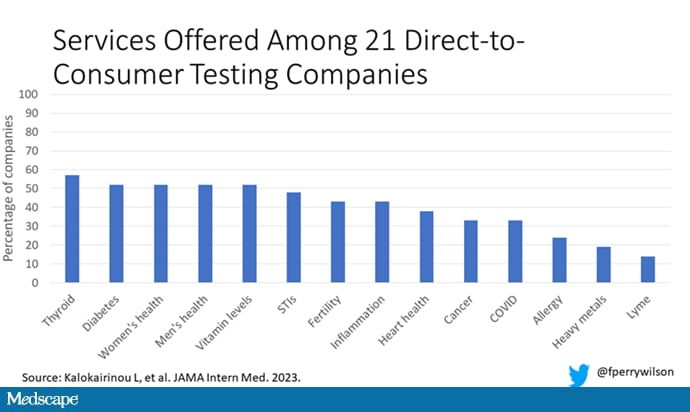
The study characterizes a total of 21 direct-to-consumer testing companies. They offer a variety of services, as you can see here, with the majority in the endocrine space: thyroid, diabetes, men's and women's health. A smattering of companies offer more esoteric testing, such as heavy metals and Lyme disease.
Who's in charge of all this? It's fairly regulated, actually, but perhaps not in the way you think. The FDA uses its CLIA authority to ensure that these tests are accurate. The FTC ensures that the companies do not engage in false advertising. But no one is minding the store as to whether the tests are actually beneficial either to an individual or to society.
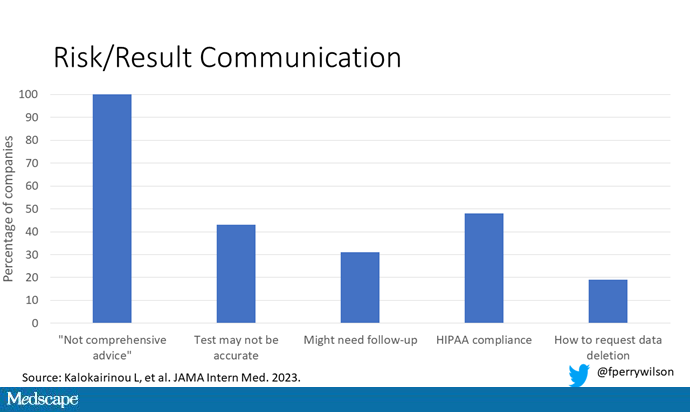
The 21 companies varied dramatically in regard to how they handle communicating the risks and results of these tests. All of them had a disclaimer that the information does not represent comprehensive medical advice. Fine. But a minority acknowledged any risks or limitations of the tests. Less than half had a statement of HIPAA compliance. And 17 out of 21 provided no information as to whether customers could request their data to be deleted, while 18 out of 21 stated that there could be follow-up for abnormal results, but often it was unclear exactly how that would work.
So, let's circle back to the first question: Should a healthy person be able to get a laboratory test simply because they want to? The libertarians among us would argue certainly yes, though perhaps without thinking through the societal implications of abnormal results. The evidence-based medicine folks will, accurately, state that there are no clinical trials to suggest that screening healthy people with tests like these has any benefit.
But we should be cautious here. This question is scienceable; you could design a trial to test whether screening healthy 43-year-olds for testosterone level led to significant improvements in overall mortality. It would just take a few million people and about 40 years of follow-up.
And even if it didn't help, we let people throw their money away on useless things all the time. The only difference between someone spending money on a useless test or on a useless dietary supplement is that someone has to deal with the result.
So, can you do this right? Can you make a direct-to-consumer testing company that is not essentially a free-rider on the rest of the healthcare ecosystem?
I think there are ways. You'd need physicians involved at all stages to help interpret the testing and guide next steps. You'd need some transparent guidelines, written in language that patients can understand, for what will happen given any conceivable result — and what costs those results might lead to for them and their insurance company. Most important, you'd need longitudinal follow-up and the ability to recommend changes, retest in the future, and potentially address the cost implications of the downstream findings. In the end, it starts to sound very much like a doctor's office.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, How Medicine Works and When It Doesn't, is available now.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Image 1: F. Perry Wilson, MD, MSCE
Image 2: F. Perry Wilson, MD, MSCE
Medscape © 2023 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Laboratory Testing: No Doctor Required? - Medscape - Sep 19, 2023.








Comments