This transcript has been edited for clarity.
Christopher J. Chiu, MD: Welcome back to The Cribsiders. This is a Medscape video recap of one of our recent podcasts. Jessica, what topic are we reviewing today?
Jessica Hane, MD, MPH, MBA: Today we're talking about pediatric brain tumors. We recently chatted with Dr Trent Hummel, a pediatric neuro-oncologist, about when to consider the brain tumor diagnosis, what to do for workup and treatment, as well as how to approach these difficult conversations with families.
Chiu: As pediatricians, we never really want to miss a diagnosis, but I think a brain tumor in particular is a diagnosis we're all a little afraid of missing. What are some red-flag signs and symptoms we should be looking for?
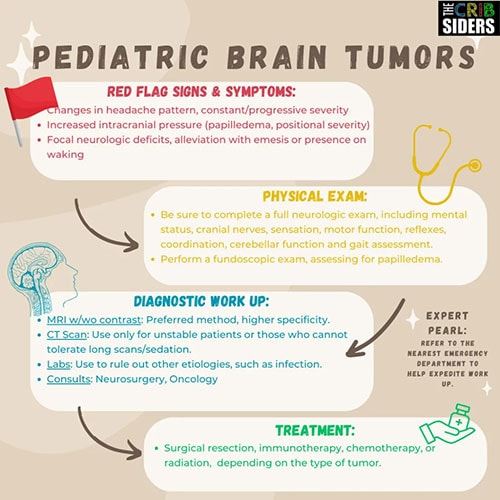
Hane: The first one that comes to mind, probably for all of us, is headache. We talked a lot about that on the podcast, particularly the specific characteristics of the headache. Worrisome headaches are those that are severe or sudden in onset. They're often persistent and progressive — the pain gets worse. Patients often complain of having pain when first waking up in the morning or positional headaches. Vomiting followed by the headache actually getting better is a big red flag for increased intracranial pressure. Other things we worry about are neurologic symptoms such as dizziness, weakness, visual changes, or frequent falls, particularly a neurologic change in addition to a headache. Those would all be red flags.
Younger kids are not always able to tell us that they have a headache, but the parents may start noticing that things are off. That parent sense kicks in. They may tell you that the child is not eating well or not acting like themselves, they are more fussy or have started vomiting (and they weren't doing that before), or that their gait has changed. He mentioned kids who were suddenly running into walls when they were previously walking well.
Chiu: Let's say we have a patient who comes in with a new-onset headache that improves with vomiting. What should we be doing during that visit?
Hane: Don't panic; fall back on your good clinical skills. Take a good history, asking about any medications they are on — for example, oral contraceptive pills or acne medications, which can cause headache. Take a good social history, asking about smoking and drug use.
Do a full head-to-toe neurologic exam, including cranial nerves, motor function, strength, coordination, gait assessment, and cerebellar function. Perform a fundoscopic exam to look for papilledema in the back of the eye, a sign of increased intracranial pressure.
If you have a high concern for a brain tumor, you should have a really low threshold for getting head imaging. Dr Hummel talked about sending patients straight to the emergency room to expedite the workup. The type of head imaging depends on the patient, the setting where you are, access to resources, and so forth, but he said that if you are putting a child under sedation to get imaging, you really should be getting an MRI with and without contrast. That's the gold standard.
Chiu: What types of treatments are we thinking about at this time?
Hane: Depending on the type of tumor, there's a huge range of treatment options. Your first step is going to be consulting neurosurgery and oncology to figure out a treatment plan. From there, for most pediatric brain tumors, total surgical resection is the gold standard. In addition to that, there may be chemotherapy, immunotherapy, and potentially radiation.
Chiu: We also brought up how to talk to families because it's a difficult subject. How do you talk to a family whose child might have a brain tumor? What were some tips from Dr Hummel?
Hane: This is really hard. I would encourage everyone to listen to the podcast to hear exactly what Dr Hummel said. He recommended using the word mass instead of cancer or malignancy when you're breaking the news. It's a word that most people tend to understand. And we don't yet know all the details. We can see that it's a mass from imaging, and we may have guesses as to what type of tumor it is, but we don't always have all that information initially. We can talk about how the mass has been affecting the child. It's what has been causing the vomiting, headaches, and other symptoms.
In general, Dr Hummel encouraged us to be very careful with language. He hardly ever uses the word benign because people understand that to mean that it's not cancer. But honestly, well-differentiated tumors, even if they're slow growing, cause significant symptoms and those kids still need treatment and surgery and all that. So benign isn't really the most accurate description of what's going on.
Chiu: Do you have any other favorite pearls from our podcast with Dr Hummel?
Hane: Yes. I always like to point out what's different between the pediatric and adult populations. For kids, radiation is a last-line treatment due to its impact on the developing brain. Radiation can have other consequences for kids, including endocrine effects such as growth and thyroid hormone abnormalities. It can also affect their future reproductive potential. For these reasons, it's not used as often in pediatrics.
Chiu: Excellent. Thank you for watching this video recap of a recent Cribsiders podcast. You can download the full episode on any podcast player or check out our website.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Image: The Cribsiders
© 2023 WebMD, LLC
Cite this: Pediatric Brain Tumor: A Diagnosis You Don't Want to Miss - Medscape - Sep 28, 2023.













Comments