Abstract and Introduction
Abstract
Introduction: A variety of NPWT products have become commercially available in the last 30 years. Utilizing advanced wound therapies appropriately can improve patient outcomes and decrease health care expenditures. Due to the increasing number of available product options, Hurd and colleagues published 10 Consensus Statements and a clinical decision tree to provide guidance on how and when to use NPWT and when to transition between device types.
Objective: To demonstrate the applicability of the consensus panel's statements and the clinical decision tree, 2 clinicians in the United States and Canada explored the benefits of applying these recommendations into their routine wound management practice.
Materials and Methods: Case studies were collected and reviewed in accordance with the Consensus Statements and clinical decision tree.
Results: Case presentations illustrate the application of the consensus panel's guidance through the prescribing of the NPWT products utilized as standard of care within both facilities.
Conclusion: Utilizing NPWT devices according to the consensus panel recommendations and the clinical decision tree may assist in optimizing care delivery to patients and address logistical and economic efficiencies.
Introduction
Acute and chronic wounds create a substantial burden for patients, providers, and health care systems. In the United States in 2014, approximately 8.2 million people (roughly 15% of the Medicare population) suffered from chronic wounds.[1] Treatment of these wounds carried an estimated annual cost of between $28.1 billion and $96.8 billion to the US health care system.[1] In Canada, 50% of nursing visits in the community setting involve wound care delivery, and 35% of persons receiving community care have a chronic wound.[2,3] Because of this, Canadian provinces developed focused initiatives to improve patient outcomes, reduce hospitalizations and readmissions, and cut health care costs related to wounds. It has been estimated that adoption of these best practices could reduce Canadian community wound care costs by up to 50%.[4]
Ensuring that advanced wound therapies are utilized appropriately can improve patient outcomes and decrease health care expenditures. In the time since NPWT became commercially available in the late 20th century, it has been embraced by the medical community as a standard treatment modality for complex wounds. NPWT was initially prescribed by clinicians for the management of large, complex wounds with high levels of exudate.[5] However, a developing understanding of the multimodal mechanism of action of NPWT has expanded its application to address a range of acute and chronic wound types, regardless of their size or level of exudate.[6]
Two main categories of NPWT exist: tNPWT and sNPWT. The original systems, now categorized as tNPWT, utilize a non-disposable pump that delivers subatmospheric pressure to the wound bed. This is accomplished by the creation of an airtight seal on the periwound area with a clear, adhesive drape. Negative pressure is delivered via tubing from the pump to the wound bed through a wound filler, typically gauze or foam, and a disposable canister collects exudate from the wound. It is understood that a wide range of pressure settings deliver therapeutic outcomes, and tNPWT pumps typically provide a range of therapy modes, therapy set points, and cycle times that allow individualized care of wounds and patients.[7] sNPWT emerged on the market in the early 2000s and applies subatmospheric pressure to the wound through a smaller and more portable single-use pump. Various sNPWT systems are now commercially available and may function with or without an associated canister and integrated dressing.
In response to the numerous NPWT product options that now exist, the need arose for expert guidance on the appropriate product use to optimize clinical, economic, and logistical outcomes, as well as patient experience. In 2020, an international consensus panel of 8 experts from Canada, Spain, the United Kingdom, and the United States convened virtually with the aim of establishing a consensus on how and when to use NPWT, as well as when to transition between tNPWT and sNPWT devices.[7] Ten Consensus Statements (Table 1) were agreed upon by the panel in the following categories: therapeutic goals, wound-related factors, patient satisfaction and quality of life, care setting-related factors, economic-related factors, and NPWT system-related factors.
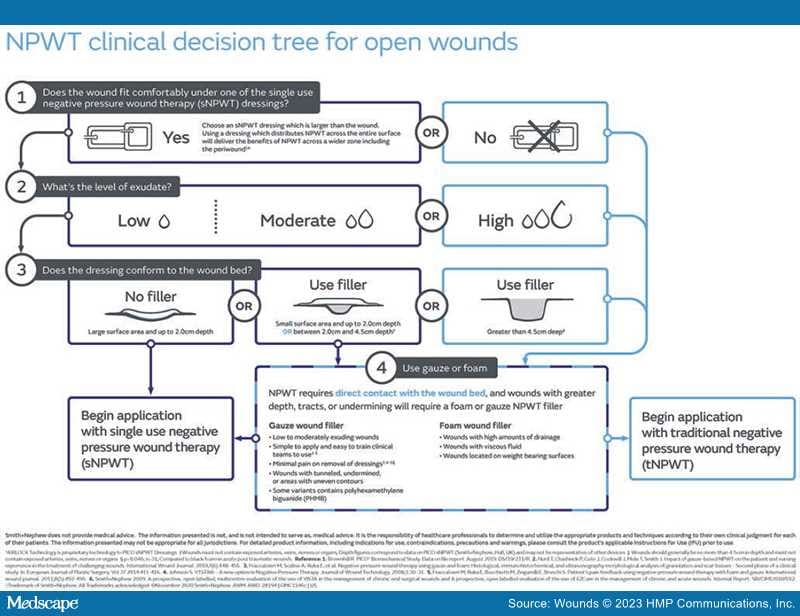
In addition, the consensus panel created a clinical decision tree to guide the selection of tNPWT and/or sNPWT (Figure 1). Both tNPWT and sNPWT operate with unique characteristics and the consensus panel recommendations, along with the clinical decision tree, guide clinicians to utilize the most appropriate therapy type.
Figure 1.
NPWT clinical decision tree for the treatment of open wounds.7
Abbreviation: NPWT, negative pressure wound therapy.
Wounds. 2023;35(7):E209-E217. © 2023 HMP Communications, LLC