Abstract and Introduction
Abstract
Introduction: DFUs are challenging chronic wounds that are vulnerable to infections. A fluorescence imaging device was developed to detect bacterial presence in wounds. This device utilizes the principle that when illuminated by violet light, some bacteria emit red fluorescence and others, such as Pseudomonas aeruginosa, emit cyan fluorescence. Several studies have reported the accuracy of this device. However, to the best of the authors' knowledge, no studies have examined the correlation between bacterial presence and tissue biopsy culture results in diabetic wounds.
Objective: This study aimed to investigate the diagnostic accuracy of a fluorescence imaging device using a tissue culture system.
Materials and Methods: Thirty-five patients (48 wounds) were included. Wounds were sampled using tissue culture methods and photographed using the fluorescence imaging device. Culture outcomes were categorized into non-Pseudomonas bacterial, Pseudomonas bacterial, both bacterial, and no-growth groups. Image outcomes were categorized into red, cyan, both colors, and negative groups.
Results: For detecting the presence of bacteria, the fluorescence imaging device showed a sensitivity, specificity, PPV, and NPV of 64.1%, 55.6%, 86.2%, and 26.3%, respectively, with an accuracy of 62.5%. For P aeruginosa, the device showed a sensitivity, specificity, PPV, and NPV of 66.7%, 87.2%, 54.6%, and 91.9%, respectively, with an accuracy of 83.3%. For non-Pseudomonas bacteria, the device showed a sensitivity, specificity, PPV, and NPV of 43.8%, 62.5%, 70.0%, and 35.7%, respectively, with an accuracy of 50.0%.
Conclusion: The fluorescence imaging device can help to detect the bacterial bioburden; however, its accuracy may be lower than that reported in previous studies of diabetic wounds.
Introduction
DFUs are challenging chronic wounds due to their vulnerability to many factors that impair the wound healing process.[1] Although several factors are involved in delayed or nonhealing foot ulcers in patients with diabetes, infection is the most direct and important factor that influences wound healing. Even with proper management, diabetic foot infections can be difficult to control and may lead to amputation. Normally, wound infections manifest as local (eg, pain, erythema, edema, and warmth) or systemic (eg, fever and elevated white blood cell count) symptoms, depending on the severity of infection. However, these symptoms and signs may not be distinct in patients with DFUs because of their poor ability to detect bacterial invasion and diminished inflammatory responses.[2] Therefore, it is important to identify the presence of bacteria in DFUs. The gold standard for identifying the presence of bacteria in a chronic wound is tissue biopsy culture.[3] However, because of its technical difficulty and invasiveness, swab cultures have been used as alternatives in several clinical trials. Swab culture is a relatively simple and less invasive method; however, its diagnostic validity in chronic wounds is unreliable.[4] Moreover, both methods are time- and resource-consuming for bacterial culture and laboratory processes.
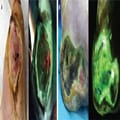
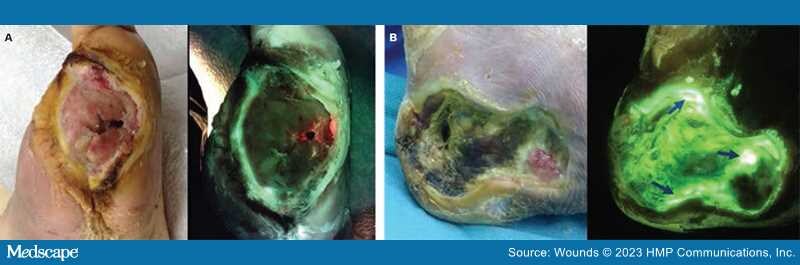
To address these limitations, a bacterial fluorescence imaging device (MolecuLight i:X, MolecuLight Inc) was developed. This device utilizes the basic principle that when illuminated by violet light (405 nm), some bacteria containing endogenous porphyrins emit a red fluorescence signal (Figure 1A), while others such as Pseudomonas aeruginosa, which produce pyoverdine, emit a cyan fluorescence signal[5] (Figure 1B). With a dim background light, this handheld device can capture real-time colored fluorescence imaging and has the advantages of being easy to learn, noninvasive, and able to provide immediate information about the presence of bacteria.
Figure 1.
(A) Red and (B) cyan fluorescence images.
Several studies have reported the diagnostic accuracy of the bacterial fluorescence imaging device;[6–16] however, some limitations exist. In most studies, specimens are collected using the swab technique. Furthermore, most studies determined the diagnostic accuracy using comparison with quantitative polymerase chain reaction, which is not commonly used in the practical clinical setting, rather than using tissue culture methods. To the best of the current authors' knowledge, no studies have been conducted on diabetic wounds alone.
The purpose of this study was to investigate the diagnostic accuracy of a fluorescence imaging device for diabetic wounds using a tissue culture system which is the gold standard for identifying the presence of bacteria. To determine this, the sensitivity, specificity, PPV, and NPV of the device were measured, and possible differences in diagnostic accuracy between P aeruginosa and non-Pseudomonas bacteria were explored. Further, the results of previous studies were investigated.
Wounds. 2023;35(7):E218-E223. © 2023 HMP Communications, LLC