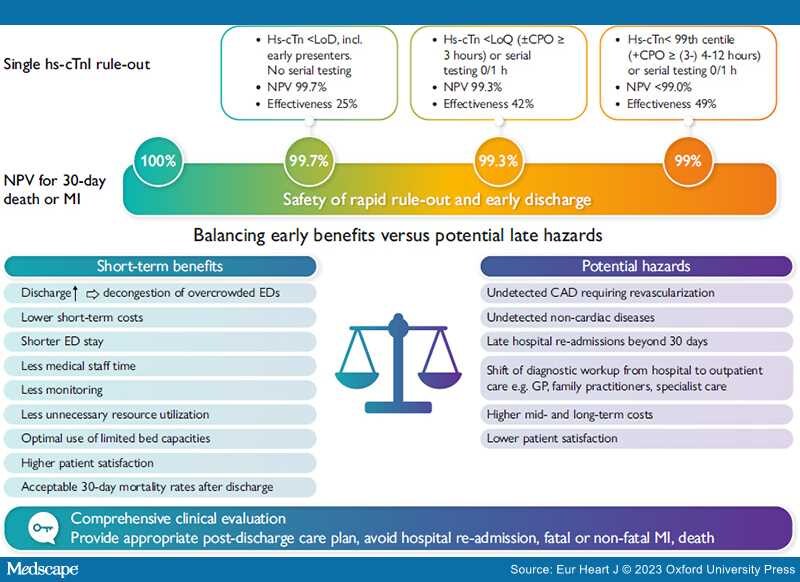
Graphical Abstract
Trade-off between early benefits and potential late hazards. 'Rule-out' is a triage category and not a diagnosis. There is a hazard for late major cardiovascular events if the reason for presentation at the Emergency Department has not been addressed appropriately post-discharge.
In this issue of the European Heart Journal,[1] Lowry and co-workers present a secondary analysis from the randomized High-STEACS trial[2] on 41 103 patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). They carefully investigated the value of a single high-sensitivity cTnI (hs-cTnI) concentration below the limit of detection (LoD) measured by the Abbott Architect hs-cTnI assay to safely rule out acute myocardial infarction (MI) in early and late presenters. The findings were tested in 7088 patients from the multi-centre APACE registry where the same cTnI assay was validated in a similar NSTE-ACS population.[3]
The investigators confirm the concept that a very low hs-cTn concentration in blood at baseline enables the 'rule-out' of MI with a sensitivity and negative predictive value (NPV) of 99.4% and 99.7%, respectively, in patients presenting <3 h from onset of symptoms to troponin testing. Not unexpectedly, discriminator sets using higher hs-cTnI concentrations such as limit of quantitation (LoQ), i.e. the concentration that can be measured with an imprecision of <10%, and the sex-specific 99th centile of the upper limit of normal (ULN) were associated with lower sensitivities and NPVs. The latter finding may be surprising, since the 99th centile is a key component of the universal MI definition.
The use of a single very low hs-cTn in 'rule-out' algorithms for MI is not novel and is part of existing triage algorithms such as the ESC 0/1 or ESC 0/2 h triage[4] and the High-STEACS protocol.[2] Nevertheless, the authors have to be congratulated for this analysis which further strongly supports the implementation of fast triage protocols in suspected NSTE-ACS.[5] The safety of the fast protocols, particularly the ESC 0/1 h algorithm, has been questioned particularly in early presenters and in patients with a history of ischaemic heart disease, diabetes mellitus, and chronic kidney disease.[5] The 2020 ESC Guidelines,[4] for example, recommend not to use a single hs-cTn concentration for 'rule-out', if chest pain onset is <3 h before troponin testing. In this context, the confirmation of high NPV of the LoD observed in High-STEACS by APACE cohorts is re-assuring—albeit unexpected—as previous evidence including findings from both author teams[2,6] had reported inferior performance of the 0 h algorithm in patients presenting within 2–3 h.
There are several points that need to be addressed before translating these encouraging results to clinical practice. First, none of the hs-cTn assays approved by the Food and Drug Administration (FDA)[7] is cleared to report to the LoD, but only to the LoQ, preventing its use in patient care in the USA. Second, only a small proportion of chest pain patients (in this study some 25%) are eligible for early 'rule-out' using a single hs-cTn result below the LoD, since many patients will present with troponin values well in the normal range and—considering the high prevalence of myocardial injury in elderly populations—also above the 99th centile (ULN). Third, although an earlier discharge may be associated with cost savings and higher patient satisfaction, the 2020 ESC guidelines[4] recommend a second hs-cTn measurement at ~60 ± 10 min after the first blood draw without waiting for reporting of the result.[8] Fourth, in patients with a history of ischaemic heart disease, diabetes mellitus, or impaired kidney function, the NPV of a hs-cTnI concentration below the LoD for 'rule-out' drops to <99%, emphasizing the need for a holistic diagnostic approach integrating symptoms, ECG, and comorbidities. Fifth, the precise determination of the exact time of onset of symptoms in clinical routine may be very challenging since symptoms of ACS patients are highly variable in quality and perception and may differ between ACS phenotypes.[9–11] Thus, the most severe ischaemic episode leading to troponin release may have occurred <1 h ago although chest pain symptoms may have started much longer ago. Furthermore, it is not easy to precisely identify the exact time of symptom onset particularly in the elderly, in women, and in patients with diabetes where symptoms may be less typical or almost absent. In previous studies, missing information on symptom onset ranged from 14% to 40% when information was extracted from medical records, which was markedly improved to 12% to 13% when structured interviews were used.[9] The ACCF/AHA task force on clinical data standards[12] attempts to provide some guidance and defines symptom onset in ACS as the point in time at which the patient first noted ischaemic symptoms lasting >10 min. In the case of intermittent symptoms, the most recent ischaemic episode of constant quality and intensity preceding hospital presentation should be recorded. Whether this recommendation is implemented in real-world settings is as yet unknown.
Sixth, although claimed in the title ('diagnosis of myocardial infarction'), the study does not present data on the performance of a single very high hs-cTnI concentration at presentation for 'rule-in' of MI. Considering the time-dependent appearance kinetics of cTn in blood, a short time interval from symptom onset to troponin testing is likely to be associated with false negatives in early presenters. Conversely, a longer time delay from onset of symptoms to troponin testing in late presenters is likely to increase specificities and positive predictive values (PPVs) for the diagnosis of NSTEMI. Finally, all observations and safety claims were based on the Abbott Architect hs-cTnI assay. Although additional performance data were provided for another six commercially available hs-cTn assays, the small number of events and incomplete information on the performance of a single hs-cTn across the entire diagnostic spectrum precludes a generalization of claims and warrants additional supportive evidence.
In summary, this study confirms in a very large patient cohort previous observations that hs-cTnI concentrations in the admission sample that are undetectable (below the LoD) by the Abbott hs-cTnI assay safely rule out patients with MI, and are associated with a very low risk for the combined endpoint MI and cardiovascular death at 30 days. The important work by Lowry and co-workers furthermore expands the evidence for the safety of the below LoD rule-out strategy also to ACS patients presenting early, e.g. within 3 h after onset of symptoms. This added information will facilitate the hs-cTn-based diagnostic work up of most patients with suspected ACS even if they present earlier than 3 h after onset of symptoms.
However, 'rule-out of MI' is not a diagnosis of a disease but a description of work in progress. Therefore, further actions beyond discharging the patient and clearing a congestion in an emergency unit must follow, that target the needs of the patients (Graphical Abstract). Subjects seeking help for distressing unknown cardiac symptoms and waiting in an unpleasant setting of an emergency department deserve a careful and comprehensive clinical evaluation and an appropriate post-discharge care planning (Graphical Abstract). This responsibility clearly goes well beyond ordering an admission high-sensitivity cTn testing and should comprise investigations for non-cardiovascular disorders as well. While we now have substantial data on acute cardiac event rates in the ACS patients sent home based on an early hs-cTn result below the LoD, we need more data on long-term re-admission rates, total mortality rates, non-cardiac mortality rates, and rates of undetected non-cardiac disease in those sent home with an hs-cTn below the LoD and a label 'MI excluded'. However, given that comprehensive medical examination will be pursued and individualized care will be provided for all patients with suspected ACS, it is very re-assuring that an undetectable cardiac Tn using a high sensitivity assay is an excellent indicator of a very low cardiac risk not only in presumably healthy populations but also—as shown here—in patients presenting early or late with suspected NSTEMI-ACS in an emergency department.
Eur Heart J. 2023;44(30):2859-2861. © 2023 Oxford University Press
Copyright 2007 European Society of Cardiology. Published by Oxford University Press. All rights reserved.