This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. I'm Dr Matthew Watto, here with my great friend, Dr Paul Nelson Williams. We are going to be talking about resistant hypertension. Is this a topic of any use to you in practice?
Paul N. Williams, MD: It comes up all the time. There's a reason we've done 35 different episodes about hypertension on the podcast. This podcast was hugely useful. Dr [Jordy] Cohen knocked it out of the park.
Watto: We're huge hypertension nerds, but I learned a lot of new stuff in this episode. Let's give everyone a little taste of it on this short video.
Some people have RAAS (renin-angiotensin-aldosterone system)-driven hypertension. Some people have extra sympathetic drive causing their hypertension. But probably everybody has a little bit of both. So Dr Cohen told us that in her practice she asks about anxiety. Is that something that you've been doing? Did that surprise you that she has a lot of luck with a certain medication?
Williams: It surprised me that there was a specific medicine that has been studied and has evidence behind it for anxiety and hypertension.
Dr Cohen works at a hypertension clinic. By the time patients get to her, they are probably in the land of resistant hypertension already. So she will screen for anxiety once they get to the point where the standard medications don't seem to be doing as much as she might expect. She suggests that if you uncover anxiety during that screening, citalopram actually has good evidence and has been very effective at lowering blood pressure in patients who have that sympathetic drive that's caused somewhat by their underlying anxiety. Citalopram seems to be the medication that is most efficacious in lowering blood pressure. I don't know about you, but I thought that was fascinating.
Watto: I thought it was fascinating too; I hadn't heard about it. She's a good primary care doctor, too, so she builds rapport with the patient first. She doesn't immediately suggest that anxiety is causing their blood pressure problem. She does her due diligence.
There was something else that she said we should check on all patients. What was that, and is it something you are now doing more in your practice?
Williams: Because of our many episodes on hypertension in the past, I've been doing it more often, but she recommends checking for hyperandrogenism. Check the patient's renin-aldosterone levels. It causes a good chunk of resistant hypertension — 20% or 30% — the number varies depending on whom you ask, but it's a good amount.
Dr Cohen made the point that a lot of people say, "Why check? It's not going to change my practice." But it turns out that in practicality, it does. Once you have the diagnosis, you're much more likely to prescribe what is probably the fourth-line agent you should be picking anyway. Having the diagnosis makes you more likely to choose something that will be a bit more helpful for the patient.
Watto: You're looking for that suppressed renin and that elevated aldosterone level. See previous podcast episodes of ours; we have episodes with some great experts on how to interpret those results.
So we're going to ask patients about anxiety, which is a new thing for me, and consider citalopram, and maybe send a renin level. Dr Cohen has a specific order for all this. With every patient, almost regardless of the etiology for their hypertension, you're going to use first-line agents, calcium channel blockers, ACEs or ARBs, and a diuretic. What was the fourth-line agent she would use most of the time?
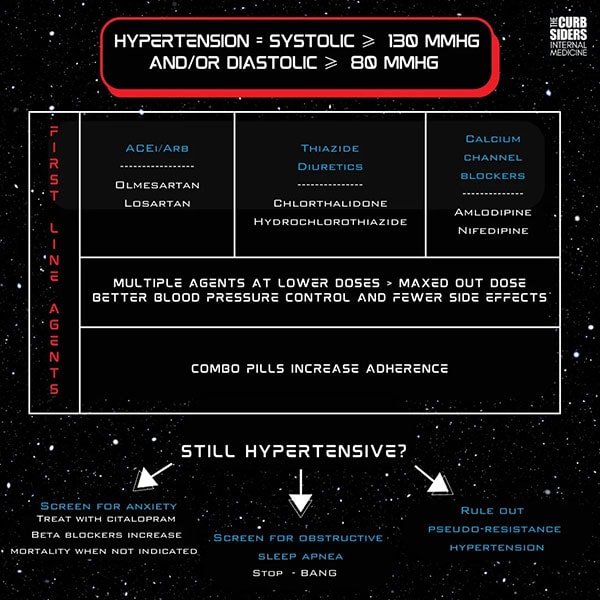
Williams: More specifically, she mentioned what it wouldn't be. It's not unusual to reach for a beta-blocker once you've kind of run out of options. It feels like it's not going to mess with the electrolytes too much. It's a medication of comfort and dosing. So I understand the impulse, certainly. But it turns out that in the absence of a hard indication for a beta-blocker, that may even worsen cardiovascular outcomes.
I was surprised to learn that Dr Cohen might even reach for guanfacine, which I had not thought much about in the past couple of years. Or she might even try the clonidine patch before she reaches for a beta-blocker in the absence of hard indication, because the outcomes seem to be worse in addition to them not typically being great antihypertensives.
Watto: I knew beta-blockers were no longer first line for hypertension, and generally I'm only using them if someone has another indication, such as atrial fibrillation systolic heart failure. There's evidence that they can even worsen cardiovascular outcomes in some populations (such as HIV patients) who don't have another indication for a beta-blocker.
So, the calcium channel blockers, ACEs, ARBs, and diuretics are your first three agents. If you are going to add a fourth agent in someone with either suppressed renin or hyperaldosteronism, amiloride is an option she might consider if the patient can't tolerate a mineralocorticoid receptor antagonist because of side effects. And as you said, guanfacine or clonidine patches (not the pills), because the patches provide a steadier drug level.
There was a lot of great stuff on this episode, Resistant Hypertension, so click on the link to hear the full podcast with Dr Jordy Cohen.
Follow Medscape on Facebook, X (formerly known as Twitter), Instagram, and YouTube
Credits:
Images: The Curbsiders
© 2023 WebMD, LLC
Cite this: Matthew F. Watto, Paul N. Williams. Resistant Hypertension: What Not to Reach For - Medscape - Sep 28, 2023.











Comments