

Why the 5-Day Isolation Period for COVID Makes No Sense
New research suggests that the recommended 5-day isolation period for patients with COVID-19 is too short. Five days is the length of time recommended for isolation by the CDC, which cut that time from 10 days and eliminated a requirement for a negative antigen test to end isolation.
Many individuals are symptomatic, and many people test positive long after that point, Yale School of Medicine's F. Perry Wilson, MD, MSCE, said in a Medscape commentary. Wilson pointed to a study in JAMA Network Open of 248 vaccinated student athletes with COVID-19 at an NCAA Division I school who were put into 7-day isolation and given antigen tests at the end of that period.
The results: Some 27% of the athletes tested positive in an antigen test after isolation for 7 days.
Testing positive: More than half of those positive on day 7 tested positive again on day 8, and more than half of those tested positive again on day 9. By day 10, they were released from isolation without further testing.

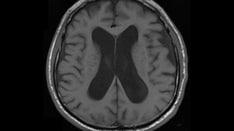
No Effect of Diet on Dementia Risk?
A healthy diet, including the Mediterranean diet, does not reduce dementia risk, according to new research. The study in Neurology contradicts prior studies into dietary habits and their effect on dementia risk, which had inconsistent results.
The study looked at 28,025 adults without dementia over a 20-year period as part of the Swedish Malmö Diet and Cancer Study. Researchers assessed food habits from 7-day food diaries, questionnaires, and interviews.
No association: The study found no association between healthy diets and the future risk for dementia or beta-amyloid accumulation after adjusting for demographic and other lifestyle factors.
Risk factors: Those who developed dementia were older, had a lower level of education, and had more cardiovascular risk factors and comorbidities.

Addiction Drug Shows Promise in Lifting Long COVID Brain Fog, Fatigue
Researchers are looking at a drug used to treat addiction to see if it can treat long COVID, Reuters reports. Naltrexone, a generic drug typically used to treat alcohol and opioid addiction, has also been used to treat patients diagnosed with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), a complex postinfectious syndrome marked by cognitive deficits and overwhelming fatigue that is similar to long COVID.
At least four clinical trials are planned to test naltrexone in hundreds of patients with long COVID, according to a review of Clinicaltrials.gov and interviews with ME/CFS and long COVID researchers.
Short listed: The drug is on the short list of treatments to be tested under the US National Institutes of Health's $1 billion RECOVER Initiative, which aims to uncover underlying causes and find treatments for long COVID.
Why it's promising: Naltrexone has anti-inflammatory properties and has been used in low doses for years to treat conditions such as fibromyalgia, Crohn's disease, and multiple sclerosis.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube
© 2022 WebMD, LLC
Send comments and news tips to news@medscape.net.
Cite this: COVID-19 Study Undercuts 5-Day Isolation; Diet Doesn't Reduce Dementia Risk; and New Hope for Patients With Long COVID - Medscape - Oct 19, 2022.






Comments