Case Presentation
A 54-year-old white man presented with generalized weakness and lower extremity swelling. He also had an ulcerated umbilical mass.
The patient has a long history of intravenous drug abuse and heavy alcohol use. Several years ago he was told he had chronic liver disease due to hepatitis C and alcohol abuse. He has never had any known complications of cirrhosis. One month ago, the patient noted a painful, ulcerated papule in his umbilicus. Three weeks ago, his lower extremities and abdomen began to progressively swell. About that time intermittent melenic stool developed. For 2 weeks, he had weakness and malaise. He sought medical attention because of progressive abdominal distension, increased size of the umbilical ulcer, and extreme fatigue.
A review of systems is negative for fever or night sweats. There is no dysphagia, odynophagia, dyspepsia, nausea, vomiting, diarrhea, constipation, abdominal pain, hematemesis, or hematochezia.
He has had no hospitalizations, operations, or serious medical illnesses other than chronic liver disease. He takes no medications.
The patient is unemployed and lives in a motel. He has been estranged from his family for many years. There is no history of travel or exposures to infections or toxins. He is a long-time user of tobacco, cocaine, intravenous drugs, and alcohol. His father died of myocardial infarction and his mother died of cancer of uncertain type.
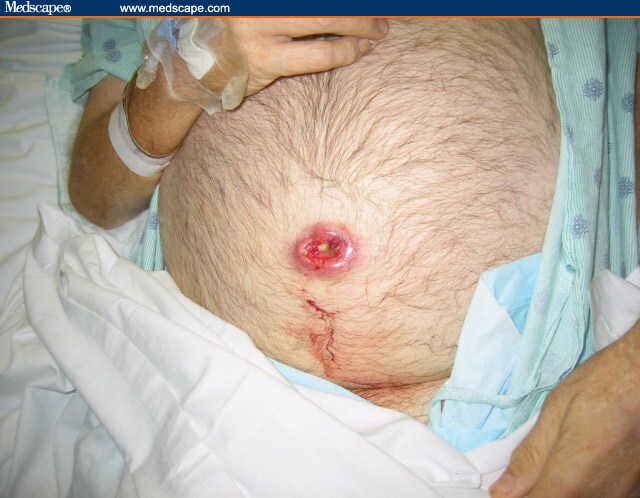
Physical examination revealed obvious ascites but no acute distress. The vital signs were normal except for a blood pressure of 94/71 mm Hg. There was no jaundice or scleral icterus. There were no spider angiomata, palmar erythema, enlarged parotids, or gynecomastia. Abdominal examination showed a grossly distended, nontender abdomen with a fluid wave and shifting dullness. The liver and spleen were not palpable. The patient's umbilicus was replaced by a 3 by 3 cm ulcer with erythematous, raised, indurated borders and a necrotic center (Figure 1). There was no discharge or purulence.
Figure 1.
Laboratory studies revealed the following:
Hemoglobin: 6.8 g/dL;
Mean corpuscular volume: 85 fL;
White blood cell count: 16,600 cells/mcL;
Platelets: 385,000 cells/mcL;
International normalized ratio: 1.2;
Total bilirubin:1.7 mg/dL;
Direct bilirubin: 1.4 mg/dL;
Alkaline phosphatase: 766 U/dL;
Aspartate aminotransferase: 103 U/dL;
Alanine aminotransferase: 66 U/dL;
Albumin: 1.8 mg/dL;
Iron: 10 mcg/dL;
Total iron-binding capacity: 338 mcg/dL (percent saturation 3.0); and
HIV antibody: negative.
Diagnostic Question
On the basis of the findings reported above, which of the following disease processes do you think is responsible for this patient's clinical presentation?
Infectious
Autoimmune
Neoplastic
Dermatologic
Congenital/embryologic
Reader Comments on: A Man With an Umbilical Ulcer
See reader comments on this article and provide your own.
Readers are encouraged to respond to George Lundberg, MD, Editor in Chief of The Medscape Journal of Medicine, for the editor's eyes only or for possible publication as an actual Letter in the Medscape Journal via email: glundberg@medscape.net
Medscape J Med. 2008;10(1):11 © 2008
Medscape
Cite this: A Man With an Umbilical Ulcer - Medscape - Jan 15, 2008.





Comments